“The global COVID-19 pandemic has heightened the importance of the relationship between medical practitioners and engineers,” – Soyoung Kang
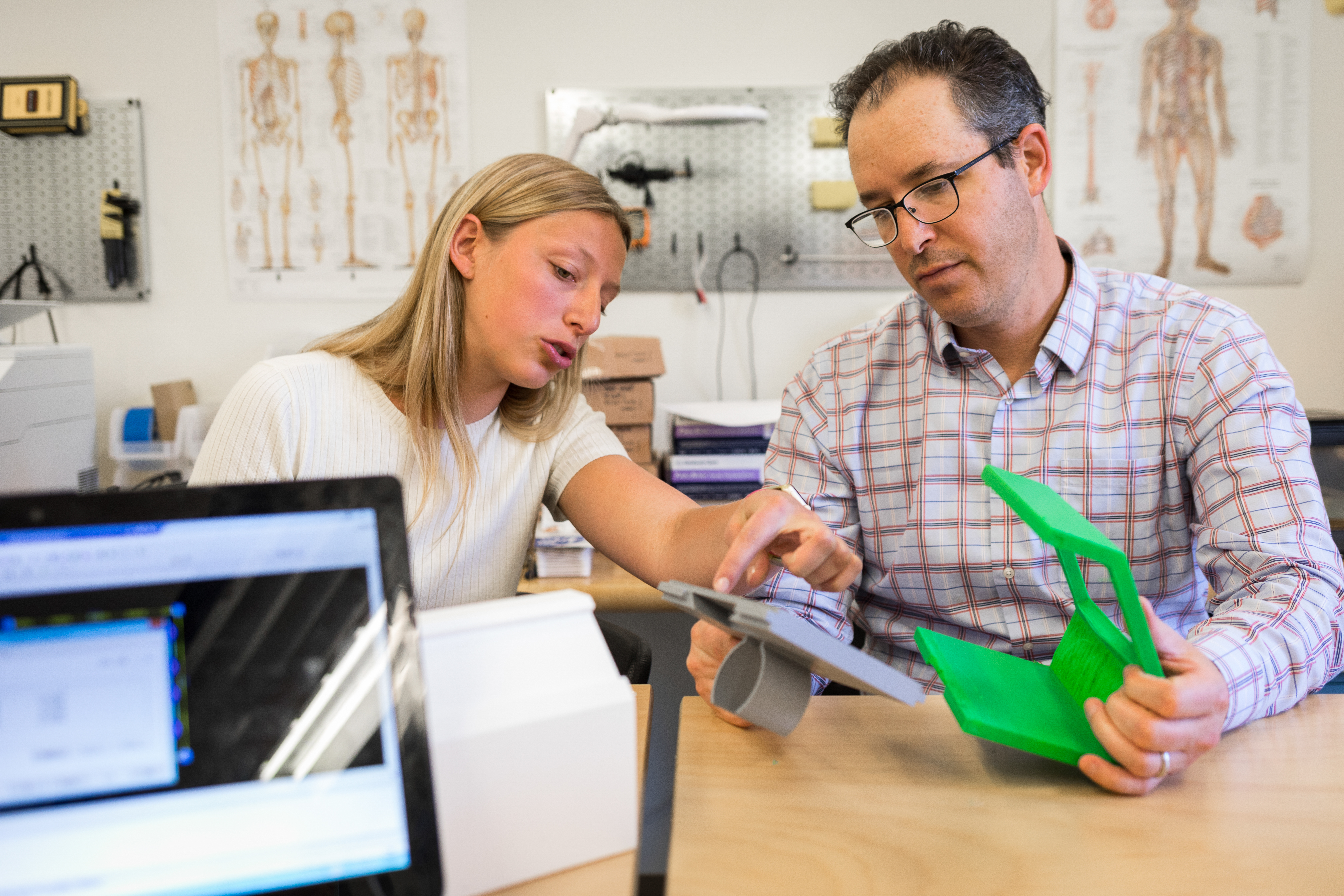
Engineering Innovation in Health brings together health care professionals with engineering students and faculty to develop solutions to today’s health challenges. Here, EIH director Jonathan Posner, right, reviews a student’s medical device prototype. Photo by Mark Stone / University of Washington
The global spread of COVID-19 has brought health care to the front and center of society’s challenges. While some engineers have pivoted their work to confront coronavirus head on, others are approaching existing health care problems that the global crisis is calling new attention to.
“COVID-19 has created many challenges for our health care system and clinicians are coming to us to develop technical solutions to those unmet needs,” says ME and chemical engineering professor Jonathan Posner.
Posner, who was recently named ME’s Richard and Victoria Harrington Professor in Engineering Innovation in Health, directs the Engineering Innovation in Health (EIH) program for the UW. Entering its eighth year, EIH has become a rallying point for connecting health care experts with problem-solving engineering students and faculty. The program asks clinicians to propose unmet health-related needs and selects the most promising ones for a team of engineering students to tackle.
The program ends with a capstone project requiring the students to build a functional prototype and has already resulted in more than 43 prototype medical devices. Some projects stop there, but many of the best move to commercialization.
“The global COVID-19 pandemic has heightened the importance of the relationship between medical practitioners and engineers,” says EIH executive director and ME teaching professor Soyoung Kang. “We’ve been thrust into a situation that’s underscoring to the entire world the need for innovation. It’s extremely motivating to everyone in our program and I believe will lead to some very important advances.”
Three projects with their origins in EIH exemplify the potential for engineering inventions that, if successful in prototyping, clinical trials and the marketplace, could improve care and save lives:
InstaQTc: Peace of mind for prescriptions
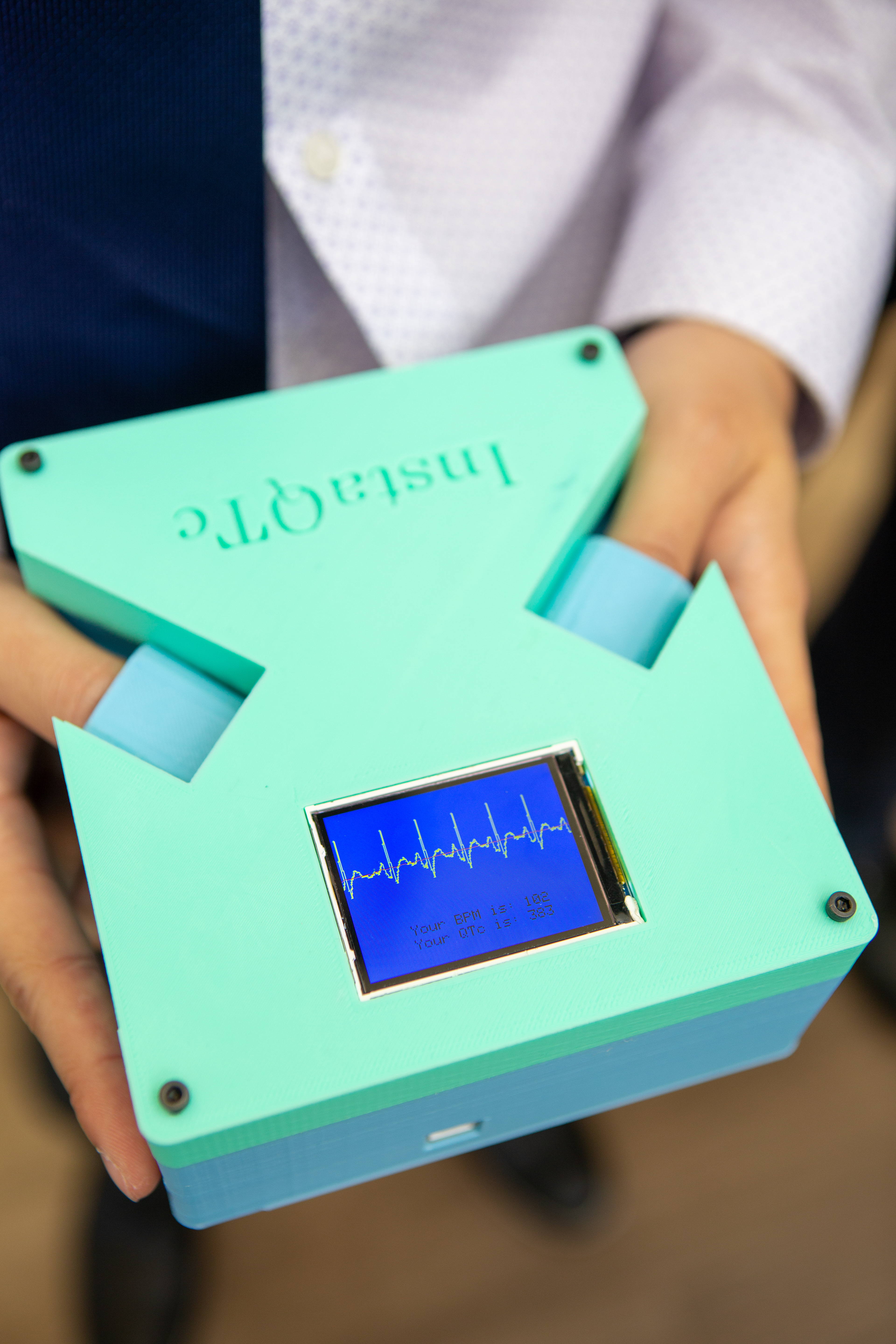
To use the InstaQTc a person simply touches its sensors and it provides a fast, accurate readout of heartrate and QT interval. Photo by Matt Hagen / University of Washington
The QT interval is an electrical measurement of the heart captured by electrocardiogram (EKG) machines. When the heart slows down and the interval gets longer, risk of irregularities in the patient’s heart rhythm increase. If the QT interval gets long enough, it leads to ventricular fibrillation and a cascade of heart-related conditions.
In the case of COVID-19, QT intervals entered the spotlight as doctors raced to test various drug treatments. With many medications, monitoring the QT interval serves as a key indicator of safety and is one of the reasons the FDA cautions against a controversial malaria drug called hydroxychloroquine for treating COVID-19.
Among the most promising devices to come out of EIH, InstaQTc measures QT intervals. By touching the InstaQTc’s simple sensors, the device reads the QT measurement and makes it easy to monitor for heart irregularities.
While hospitals won’t be doing away with their EKG machines any time soon, many health care clinics don’t have access to EKG machines, such as urgent care or those that are remote, rural or in developing world settings. Psychiatrists also don’t typically have EKG machines and could use an InstaQTc to reduce the risk of prescribing new medications.
Valley Medical Center faculty physician Jon Neher, who introduced the idea for InstaQTc to EIH, says it came to him while listening to family medicine physicians discussing a research protocol that required them to send numerous patients for EKGs just to get a QT interval reading.
“I thought, ‘That is really a cumbersome way of doing this, there’s got to be a better way,’” recalls Neher. “But it turned out there wasn’t a good way, and that’s what prompted me to think maybe EIH could help me develop something.”
Neher was paired with Kang and a team of four undergraduate students: Nanye Du and Trinh Vo from ME, Marissa Shibuya from electrical and computer engineering (ECE) and Hengjia Zhu from materials science and engineering (MSE). The team began work on the project in the fall of 2018 and after all four graduated in 2019, Vo and Du continued to develop the project as a commercial venture, first through the EIH summer incubator and then as graduate students.
“The prototype has been through many, many iterations already,” says Vo. “The prototype we’re working on now is probably the 20th or 30th version.”
InstaQTc has been supported through UW CoMotion with an Innovation Gap Fund award. The team has also received a provisional patent, approval for clinical testing in two locations, including Neher’s clinic, and is engaging with NSF I-Corps on market research.
Sensit-IV: Taking the guesswork out of giving fluids
Before becoming a surgical fellow at UW Medicine, Catherine Beni got her Ph.D. in applied mathematics (the youngest woman ever to receive a Ph.D. from Caltech). So it may be no surprise that she’s always looking for ways to introduce more quantification and precision into medicine.
“As someone that has to order IV fluids a lot, I never know exactly how much to give, at what rate to give it, when to stop, or whether I might even be doing more harm than good,” says Beni. “We don’t actually know what the rate of leakage is and it’s kind of a guessing game.”
Ordering intravenous (IV) fluids for patients who have low blood pressure is one of the most common medical interventions worldwide. The “leakage” referenced by Beni is a phenomenon known as capillary leak, where the fluids leak from the veins into the surrounding tissue. Capillary leak is particularly common when a patient has experienced a significant physical trauma and the body opens capillaries to allow white blood cells in to treat the injury.
The fluid leakage is a major problem. Beni says 1.2 million people go to intensive care units in the United States each year from loss of blood or severe infection, and reducing one day of intensive care for just these patients would result in over $5 billion of savings. Additionally, a third of the patients are discharged with excess fluid weight, which causes a cascade of other costs, including follow-on treatments, physical therapy and delays in the ability to return to work.
In the case of COVID-19, capillary leakage carries a unique threat due to the SARS-CoV-2 virus infecting the respiratory system. Because capillaries need to be very close to air sacs in the lungs to allow oxygen into the blood stream, fluid leakage can easily happen the other direction, causing fluids to build up in the lungs and preventing the patient from being able to get oxygen.
The goal of Sensit-IV – the project the Beni proposed to EIH – is to take the guesswork out of IV fluids through a custom-designed monitor that guides IV fluid management. Beni was paired with Posner and a team of engineering students including Aman Garg, Nelson Warner and Syndey Yeh of ME and Kenneth Shim of ECE.
Like InstaQTc, Sensit-IV has received a CoMotion Innovation Gap Fund award and is participating in the 2020 EIH summer incubator. Beni and the student team will continue developing their device in the coming year.
EAGER: UV sterilization for ventilator breathing tubes
“My presumption is he had a 14-day quarantine, and for someone used to working 90 hour weeks, that’s a lot of time to think about how to fix a problem that’s bothering you,” conjectured ME professor Eric Seibel on the origins of his recent partnership with Jacob LoMonaco.
LoMonaco, who finished his rounds as a surgical resident at UW Medicine this spring and is now an emergency medicine resident at University of Nevada Las Vegas, was specifically thinking about the problem of patients catching pneumonia as a result of spending too much time on a ventilator. The condition, known as Ventilator Associated Pneumonia (VAP), occurs when bacteria colonize the surfaces on and around the breathing tube that’s inserted into a patient’s windpipe.
Much like unbrushed teeth, the bacterial biofilms worsen the longer they’re left to grow and eventually lead to pneumonia. And though there are many reasons a patient may need to be put on a ventilator, COVID-19 has caused a huge spike in ventilator usage, leading to corresponding reports of VAP complications.
LoMonaco wondered whether bright UV light shined down into the ventilator tube could reduce biofilms, like optically brushing your teeth. Hospitals routinely use UV to kill microbes on other medical equipment, so he reasoned a ventilator tube might be no different. He reached out to CoMotion, who connected him to EIH and to Seibel, an expert in catheter-sized medical optics and photonics.

Professor Eric Seibel, center, is a research professor in ME. He has been involved with EIH since the program began in 2013. Photo by Mark Stone / University of Washington
LoMonaco and Seibel prepared a proposal for their device, which NSF awarded with an exploratory grant. Seibel and his team are now building a prototype based on their design and will test its effectiveness.
The tip of the iceberg
There are many uncertainties going into this fall at UW, but one thing is clear: it’s more important than ever for engineering researchers to continue working diligently with medical experts to address health care outcomes. InstaQTc, Sensit-IV and EAGER represent just a few of the many promising projects being undertaken by EIH.
The program is accepting proposals for the coming year and encourages clinicians to submit ideas via their short Clinical Project Application.
Whether you’re a clinician, student or industry professional, visit Engineering Innovation in Health or email eihealth@uw.edu to learn more about the program and how to get involved.
Originally published August 6, 2020
