By Lyra Fontaine
ME students and faculty partner with UW Medicine to create devices that can treat multi-organ failure and improve catheter safety.
Collaborations between mechanical engineers and UW Medicine are creating new health-care possibilities. When ME researchers partner with UW Medicine through programs such as Engineering Innovation in Health (EIH), which promotes interdisciplinary collaboration between engineering and the health sciences at the UW, they create innovative solutions to pressing unmet health challenges.
What’s more, the projects equip students with valuable engineering and entrepreneurship skills. After researching the need and developing a solution, students learn about commercialization processes for their device. UW startup resources at CoMotion and the Buerk Center for Entrepreneurship support them along the way so they can take their technical solutions to the next level.
Recently, ME students and faculty developed devices that improve care for people with multiple organ failures and for individuals who use urinary catheters.
AMOR: Treating individuals with multiple organ failures
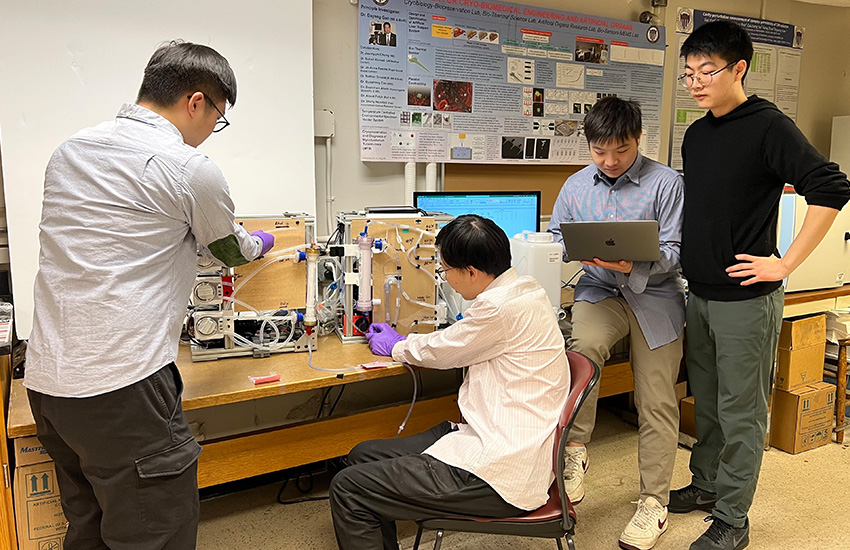
From left to right: Graduate student Nanye Du, research engineer Ye Jin, research engineer Ziyuan Wang and Ph.D. student Shaohang Hao working on the AMOR machine, which is meant to treat organ failure by removing toxins in patients’ blood. Photo courtesy of Shaohang Hao
A vital organ can fail during conditions such as sepsis and due to genetic or environmental reasons. If it’s not treated in a timely manner, a single-organ failure can quickly trigger dysfunction in other organs. Multi-organ failure is the leading cause of mortality for intensive care patients, says Dayong Gao, Professor of Mechanical Engineering.
“This urgent medical need is the major driving force for our team to develop a machine that can replace multiple vital organs’ functions,” says Gao, who co-founded the Artificial Multi-Organ Replacement (AMOR) system with Dr. Suhail Ahmad, a UW Medicine professor. AMOR became an EIH project in 2022-23, enabling undergraduate students to contribute to the device’s innovation.
AMOR treats organ failure by removing toxins in patients’ blood. If the organs can’t be repaired, the system keeps patients alive while they wait for a transplant. AMOR may also be able to help sustain people’s lives after transplantation, before the new organ is functional. The machine can be used for both urgent cases and chronic kidney/liver disease.
Device effectively treated multiorgan failure
Results from a pilot study, recently published in the Journal of American Society for Artificial Internal Organs, detail how AMOR successfully rescued individuals from multiorgan failure.
The system supports several organs at the same time, focusing primarily on liver and kidney function. Unlike dialysis machines, AMOR is able to remove sufficient protein-bound toxins, as well as excess fluids from outside the bloodstream. This is important because the excess fluids can lead to swelling, pressure on organs and injury.
“AMOR was remarkably successful in removing a large amount of excess body fluid, which the regular hemodialysis machines could not achieve,” Gao says. “We believe this led to improvements in pulmonary and cardiac function.”
During the collaborative design process, the team considered effectiveness and safety, working with Ahmad’s team to understand users’ needs and parameters that could affect treatment. This included ensuring that there are no air bubbles before recirculating blood to the body.
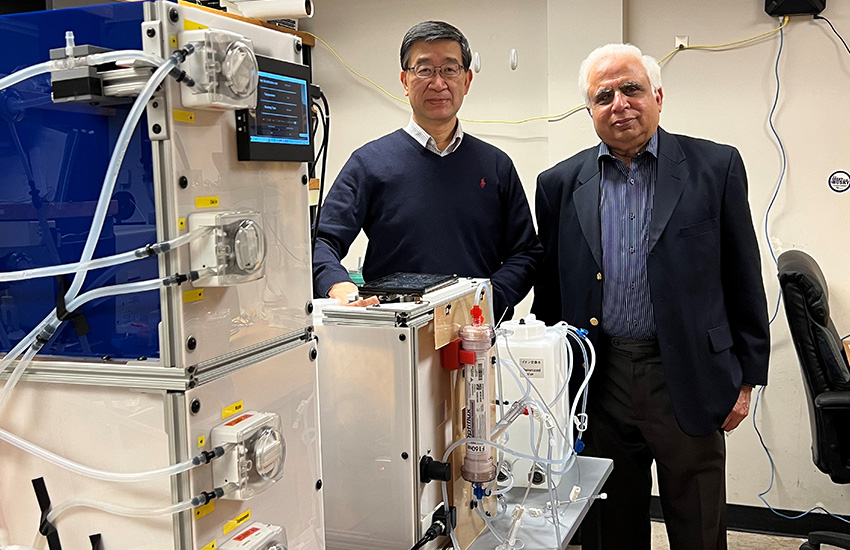
AMOR co-founders Dayong Gao, Professor of Mechanical Engineering, and Dr. Suhail Ahmad, a UW Medicine professor.
The machine removes toxins and pumps fluids back into the bloodstream. Integrated sensors can detect blood leakage, air bubbles, pressure and temperature.
“We as engineers can provide solutions to clinical problems,” says Ph.D. student Shaohang Hao. “We were able to design a system that treats multi-organ failure because we know how the mechanisms happen. For example, we know that the principle behind blood purification is mass transfer.”
Ph.D. student Alexander Novokhodko worked to optimize how AMOR purifies blood. The machine diffuses toxins, adds pressure inside the tubes to push toxins out of the bloodstream and absorbs toxins using charcoal and resin.
The researchers also automated the multi-organ failure treatment process, including fluid removal. To do this, AMOR needed more comprehensive controls. Hao led the development of the automatic control system, which integrates and automates blood pumps and sensors into the machine. Through this, he developed an automated fluid-driven platform.
In recognition of the students’ work, AMOR received second place in the Hollomon Health Innovation Challenge and the Dempsey Startup Competition in 2023. UW CoMotion has filed international patents on the technology.
“It’s been hard work, but quite rewarding,” Novokhodko says. “I’ve learned about the U.S. Food and Drug Administration (FDA) process for device commercialization, as well as making sure our device is valuable for clinicians, nurses and other stakeholders so AMOR can go from the lab to the clinic.”
The team is now optimizing the machine and participating in the rigorous National Science Foundation I-Corps program that helps startups develop their business model. The program includes interviewing clinicians about their needs to ensure the machine is user-friendly before beginning clinical trials. Previously, the team participated in a regional Innovation Corps (I-Corps) program at CoMotion.
“We hope that AMOR can be implemented around the country, including in rural hospitals, in low-resource settings and for military or emergency response,” Novokhodko says.
CathConnect: Making urinary catheters safer

The CathConnect team with prototypes of the device, which is an accessory to a catheter. From left to right: ME Ph.D. student Michael Malone (B.S. ’22), CEO Joelle Tudor (B.S. ’22), Manny Pacheco (B.S. ’20, M.S. ’22), and Chief Medical Officer Tova Weiss, MD, a urology resident physician at UW Medicine. Photo courtesy of Joelle Tudor
Nearly 1 in 4 hospitalized patients require a urinary catheter, which is a long and flexible tube used to drain urine from the bladder. However, individuals may accidentally pull on and dislodge their own medical equipment. Accidentally removing an indwelling urinary catheter can cause serious complications, including traumatic injury and increased risk of life-threatening infection.
These pervasive problems prompted UW Medicine urology resident Tova Weiss, M.D., to reach out to EIH in fall 2021. This led to a collaboration with a team of graduate and undergraduate ME students, including Joelle Tudor (B.S. ‘22) and Ph.D. student Michael Malone (B.S. ‘22), for a senior capstone project. Together they created a fully functional medical device that serves as an accessory to a catheter. Once installed, the device allows the original catheter tube to safely disconnect when pulled, protecting patients from trauma.
Traditionally, if a patient pulled out a catheter, a balloon that keeps the catheter inside the bladder may cause tissue trauma. However, the CathConnect device allows the tube to disconnect while the balloon remains inflated. It can later be reconnected for continued use. In addition to reducing injury, the innovation aims to ease the burden on caretakers and lower healthcare costs.
Tudor stepped into the world of engineering health-care in an ME biomechanics class, where she became excited to work on research that could lead to better health outcomes. CathConnect was the perfect opportunity to make an impact on healthcare.
The team kicked off the project by interviewing physicians and nurses to understand their needs. “It was great to meet people in the life sciences field and figure out ways I could make an impact with my engineering background,” says Tudor, who now leads the CathConnect spinoff company as full-time CEO. “I was able to apply my coursework to a real direct application.”

UW Medicine urology resident physician Tova Weiss demonstrates the breakaway mechanism in the device, which could reduce injury for people who use catheters. Photo courtesy of Joelle Tudor
Having both ME and clinical perspectives were essential for designing the device, which was shared with clinicians to ensure it met specific needs.
“While working with the engineering students, I would come up with an idea that wouldn’t work mechanically. Then they would propose a solution that wouldn’t work in a hospital setting,” Weiss says. “It took both of our perspectives to move forward with a solution.”
To create the device, the students used their knowledge from ME classes to design a prototype using computer-aided design (CAD). The prototype was later brought to life by 3D printing and manually assembling components.
The capstone project, and now the company, taught Tudor and Malone useful skills such as teamwork, project management, medical device prototyping and commercialization. They learned the ins and outs of regulatory approval, intellectual property and the logistics that come with starting a company.
“Evaluating the market opportunity for a particular problem, understanding the regulatory and reimbursement hurdles for new medical devices, filing for intellectual property protection and learning how to raise funds to support our commercialization efforts have been critical skills I’ve developed while working on the project,” Malone says.
CathConnect mentors included Jonathan Posner, Richard and Victoria Harrington Professor in Engineering Innovation in Health; Eric Seibel, ME research professor; and Shawn Swanson (ME Ph.D. ’23).
The project won second-place awards at the Dempsey Startup Competition and the Hollomon Health Innovation Challenge, as well as the Outstanding Design Award at the 2022 ME graduation.
Since CathConnect became a startup in 2023, the team received funding and mentorship from CoMotion, the National Institutes of Health, the National Science Foundation, VentureWell and the UW Foster School of Business Jones + Foster Accelerator. CathConnect received positive reviews at the 2023 American Urology Association Conference and won both the audience and investor vote at the 2023 Seattle Angel Conference, receiving a $207,000 investment.
Earning recognition from Forbes and the Puget Sound Business Journal, the team has come far since their original collaboration through an EIH capstone. Next steps include large-scale manufacturing development and initiating the process to receive FDA clearance. The alums and current students involved in CathConnect remain focused on improving the lives of individuals receiving medical treatment and clinicians providing care.
“With ME, there are so many different ways you can apply your degree and make an impact,” Tudor says.
Originally published January 22, 2024