By Lyra Fontaine
A first-of-its-kind medical technology, developed in part by UW Mechanical Engineering Research Professor Eric Seibel’s lab, is providing a new approach to biopsy imaging for faster breast cancer diagnoses at a hospital in Kumasi, Ghana.
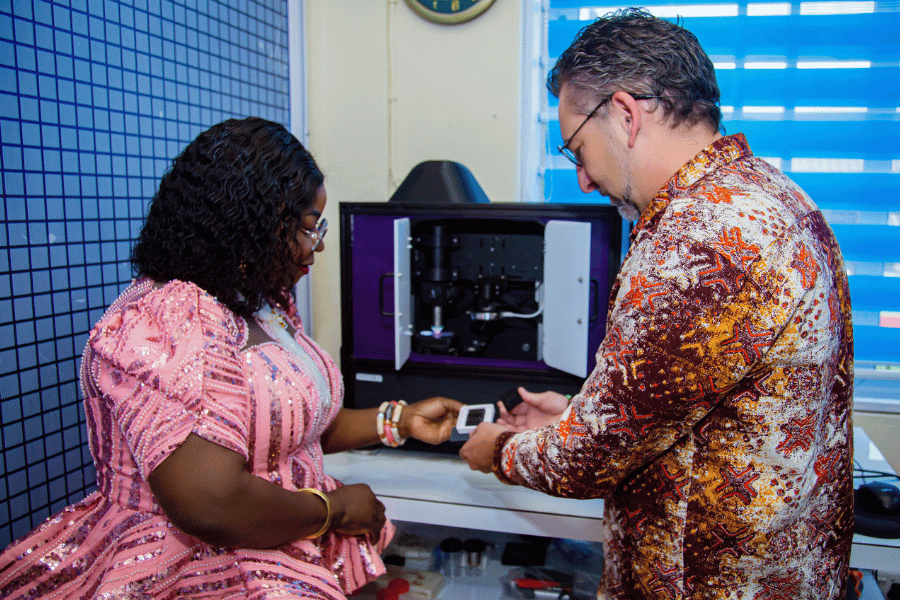
Peace and Love Hospitals CEO and consultant breast surgeon Dr. Beatrice Wiafe Addai and UW consultant Mark Fauver hold a tissue sample preparation tray, developed by the UW Human Photonics Lab. Photo provided by Addai.
In 2022, breast cancer caused about 670,000 deaths globally, according to the World Health Organization. In Ghana, breast cancer is the leading cause of cancer deaths in women. In sub-Saharan Africa, less than 40% of people with breast cancer survive five years after their diagnosis, compared to 86% in the U.S.
An early diagnosis makes it easier to successfully treat breast cancer. According to a recent study in Spain, breast cancer patients who delayed seeking medical care for more than 90 days after the beginning of symptoms were more than three times as likely to die within two years, compared with people who sought care sooner. A recent U.S. study emphasizes that for every 60-day delay between diagnosis and surgery, there is a relative 26% increase in breast cancer mortality.
However, reliable and timely testing can be a challenge for people in low- and middle-income countries due to limited availability at diagnostic centers, travel demands and socioeconomic factors.
To meet this need, the UW Human Photonics Lab, Emory University and UC Davis collaborated with Peace and Love Hospitals in Ghana to launch CoreView. The device combines a biopsy preparation tray with an imaging process that can provide diagnoses within minutes.
CoreView enables clinicians to image small tissue samples, about the size of a pencil lead, from potentially cancerous breast masses, in less than 10 minutes. Pathologists can then digitally assess the resulting image, so that the patients and clinicians can immediately know whether the mass is cancerous or not.
“This is the most fulfilling project I’ve had in 25 years,” Seibel says. “Clinicians want to use it, and it can save people’s lives. The steps are fast, reproducibility is high and we can match the gold-standard conventional pathology.”
The work is funded primarily by the National Cancer Institute at the National Institutes of Health (NIH), and prior funding from the National Science Foundation, the CoMotion Innovation Gap Fund and the Washington Research Foundation.
Faster imaging with real-time results
Clinicians in Ghana typically send tissue samples from biopsies by plane or car to various pathology labs, where pathologists might make a diagnosis within a week to several weeks.
CoreView speeds up this process. The clinician places the tissue sample into a tray, developed by Seibel’s lab for simpler tissue preparation.
.png)
The CoreView machine, which includes a tissue sample tray and microscope, at Peace and Love Hospitals in Ghana. The laptop shows the real-time images of the tissue. Photo provided by Addai.
“We pioneered the concept of having a piece of tissue in a lab-on-a-chip device,” Seibel says.
The tray helps position the tissue for imaging without manual handling. It provides a platform for the clinician to rinse the sample and apply stains within minutes.
“It’s challenging to manipulate these extremely tiny pieces of tissue, and to not lose or damage them,” Seibel says. “We’re imaging the surface, so we need to be as gentle as possible.”
Next, the clinician loads the tray onto the microscope and images the outermost tissue layers.
A type of imaging invented at UC Davis uses blue light to excite fluorescence within the tissue specimen, which is then transmitted through the stained outermost tissue layers. Imaging the surface with a microscope and camera generates images that closely resemble what pathologists are already trained to interpret. These images can be interpreted on-site or transmitted digitally anywhere in the world.
“This provides similar results to images taken the more traditional way, which involves slicing tissue and sending it to the lab, where they examine each separate slice on a glass slide with a microscope,” says UW consultant Mark Fauver, who helped develop CoreView and deliver it to Ghana.
UW researchers used design updates from the Fereidouni Lab at Emory University to build an improved clinical instrument. Fauver and Holle Lam (MSME ’25) were instrumental in developing the clinical machine and accompanying control and display software. They also tested the resulting system with users to take it from idea to impact.
“Their invaluable work was a key part of why we could deliver the device to Ghana this year,” Seibel says.
A team effort with global impact
The researchers hope that CoreView will increase patient access to breast cancer diagnoses and reduce costs. The device could be useful for pathology around the world, including in rural or under-resourced areas of the U.S. without access to nearby pathology services.
So far, clinicians have used the machine for dozens of patients at Peace and Love Hospitals. The partnership with Ghana was made possible by the American Society for Clinical Pathology’s global health outreach. Led by CEO and consultant breast surgeon Dr. Beatrice Wiafe Addai, Peace and Love Hospitals contributed their technical expertise in getting the biopsy onto the tissue preparation platform for entry into the testing protocol.
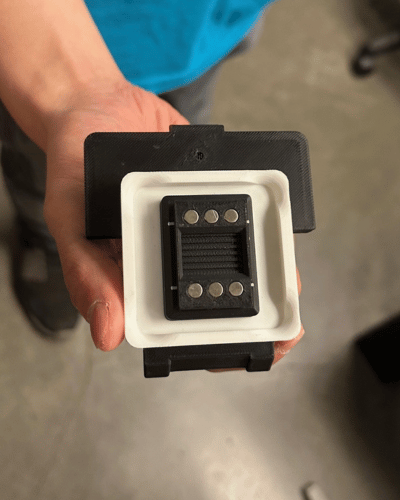
Holle Lam (MSME ’25) holds the tray where the tissue sample from the biopsy is positioned for imaging. It provides a platform for the clinician to rinse the sample and apply stains within minutes. Photo by Lyra Fontaine.
“With highly trained staff led by Beatrice, Peace and Love Hospitals is the perfect place to validate and scale up this technology, which will expand to prostate cancer diagnosis in the future,” Seibel says.
In Ghana, technicians quickly learned how to prepare the samples and image the biopsy after Fauver walked them through the process. Recently, Fauver delivered an upgraded version of the first-generation machine, with reduced sensitivity to vibration, higher resolution imaging and improved software.
“I enjoy translating research to development to make an impact outside of labs,” Fauver says. “I’m excited about what we learned from this and hope we can continue to refine the system.”
CoreView was developed by UW researchers from ME, applied physics and bioengineering. Other collaborators include Dr. Suzanne Dintzis, professor in laboratory medicine and pathology at the UW School of Medicine; Farzad Fereidouni, associate professor at Emory University; and Dr. Richard Levenson, professor at UC Davis.
In the next generation of the CoreView machine, the researchers plan to use artificial intelligence methods to detect malignant tumors, determine the type of breast cancer and help inform therapeutic decisions. Eventually, they hope to build a lower-cost, portable unit for field use.
“Our end goal is to discover the type of cancer and its molecular target for getting the patient on the correct therapy before they leave the clinic,” Wiafe-Addai says. “This is definitely a game changer in a country where late-stage presentation and diagnosis are the most important factors that contribute to the high mortality and morbidity rates.”
How you can support this research
- Donate to the Human Photonics Lab as they work on a next-generation device that enables faster and potentially life-saving breast cancer diagnoses. The team plans to further develop the device to ensure it can be used in the U.S. to find smaller masses and lesions.
- Donate to the ME External Advisory Board Endowed Graduate Student Support Fund to support graduate students working on impactful research.
Originally published October 6, 2025