December 15, 2025
Could advanced materials improve how physicians treat cardiovascular conditions like heart disease? Researchers at the University of Washington are developing medical tools designed to make vascular procedures safer and more effective.
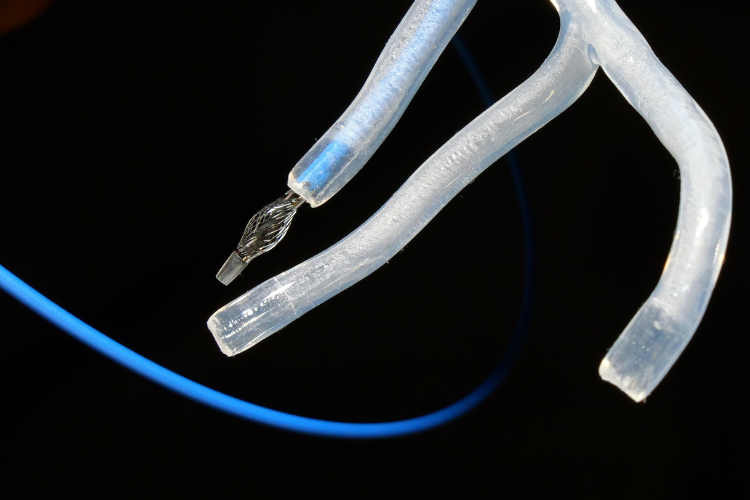
A UW team has built medical devices using metamaterials, geometry-based engineered materials that change structures when twisted. Photo provided by Aman Garg and Sawyer Thomas.
Their work addresses a pressing need: In 2023, cardiovascular disease claimed more than 900,000 lives in the U.S. Coronary artery disease, caused by plaque buildup that narrows arteries and restricts blood flow to the heart, affects about 1 in 20 adults and is the most common form of heart disease, according to the Centers for Disease Control and Prevention.
To clear blockages and restore blood flow, physicians thread thin, flexible tubes called catheters through the body's blood vessels to reach the heart. But the procedure comes with challenges. Catheters and the outer sheaths that guide them can slip out of position during surgery, potentially causing injury to the patient or bleeding.
A UW team has developed patent-pending technology that could change that. They built catheters, sheaths and endoscopes from metamaterials, geometry-based engineered materials that change structures when twisted. The devices can bend and extend to navigate through arteries and selectively expand at the tip to anchor securely in the target vessel. This stability could enable procedures to be faster, safer and more precise.
“Every second matters in endovascular surgery, and physicians are often fighting their own tools just to have safe access to the treatment site,” says Aman Garg, research engineer in ME and the project lead. “We’re building catheters that work with physicians, not against them — so they can focus on delivering the best possible outcomes for their patients.”
After scaling their metamaterial design to clinical dimensions, the researchers put the devices to the test. In benchtop simulations, their catheter navigated simulated arterial blockages and locked into place.
“Our new method gives physicians a solid foothold when advancing devices within the artery,” says ME postdoctoral researcher Sawyer Thomas (ME Ph.D. ’24, MSME ’22). “The same technology we use to expand the tube can also be tuned to perform other actions, such as extending, bending, or stiffening it.”
The team, who work with Jeffrey Lipton, a former UW ME faculty member who is now an assistant professor at Northeastern University, have applied these shape-shifting structures to robotics, bridge acoustics and aerospace. Now, in collaboration with Dr. Zachary Steinberg, an interventional cardiologist at UW Medical Center, they’re bringing that knowledge into the operating room.
“Through my time at UW, I came to realize that new materials and fabrication techniques can open up a whole new subset of design possibilities,” Thomas says. “By tuning a structure’s geometry, you can not only change its properties, but also open up a whole new set of tools.”
The technology showed promise in the lab, but the researchers needed to know if it addressed a genuine clinical need. Through the NSF National I-Corps program, they interviewed more than 100 physicians across the country, including at UW Medical Center and Harborview Medical Center, many of whom reiterated that existing devices don’t provide the stability physicians need when working inside arteries.
Taking these insights, Garg and Thomas are working to license and spin out the technology through Nimble Surgical, a medical device startup. They recently received a $314,000 National Institutes of Health (NIH) Small Business Innovation Research (SBIR) grant to support early-stage development as the team prepares for preclinical validation of its anchoring technology.
Additional support has come from the CoMotion Innovation Gap Fund, the Center for Washington Entrepreneurial Research Evaluation & Commercialization Hub (WE-REACH) and the Washington Research Foundation. The team is also participating in Life Science Washington’s mentorship program.
“Talking with physicians and watching procedures, it becomes clear how much opportunity there is to advance endovascular treatment,” Thomas says. “As tools and technology continue to evolve, I hope to see big improvements in the standard of care for patients.”